Incredible journey:
Two RVTS alumni, three kids, two dachshunds…and their path to rural practice
Husband and wife doctor team, Dr Erin Hawkey and Dr Ian Murphy, completed their advanced Rural Generalist (RG) training through RVTS and recently fellowed as FACRRMs (Ian last September and Erin in May). They now work as RGs in rural Victoria.
With a young family – Emaline (8), Gilbert (4) and Minnie (1), not to mention two dachshunds – life is busy, just as it was when they were on the RVTS pathway.
Both Erin and Ian greatly appreciated the support and flexibility provided by RVTS as they balanced their RG training, work as registrars and family life – and with a keen interest in training the next generation of doctors, they plan to remain closely involved with RVTS into the future.
They spoke about their path to Rural Generalist practice, and their RVTS experience, with Patrick Daley.

Did you have a rural upbringing?
Ian: I grew up in the small rural NSW town of Cowra. One of my friend ’s dads was a GP Anaesthetist there, so I had exposure to the rural doctor experience early on.
Erin: My family lived in Seymour, a small town about an hour from Melbourne, until we moved to Bendigo in my final year of primary school. There, I completed high school and a gap year, and maintained a rural connection via the family farm run by my mum’s parents (and later mum’s brother).
My parents and younger siblings then moved to Albury-Wodonga while I was at university doing my undergraduate science degree. Despite its size and many local specialist medical services, mum phoned more than five separate practices before she could find a general practice willing to accept new patients (and then, only privately paying ones).
Throughout my childhood, the need for high quality generalist medical services close to home was obvious to me.
What got you interested in a medical career?
Ian: I didn’t really have a clear idea of what I wanted to be until my last years of high school, when my grandfather was diagnosed with advanced lung cancer, requiring extended periods of time at the Royal Prince Alfred (RPA) Hospital in Sydney.
Seeing the way the medical staff treated him – and how the doctors would spend time talking to him and my nan about what was happening – made me want to put all my efforts into pursuing a career in Medicine.
Erin: I have always been intensely curious – particularly in nature and biological systems – and still frequently wonder ‘Why does something look or work like this?’
Playing outside as a small child, I collected worms, dug up witjuti grubs, caught butterflies and grasshoppers, played with the chooks and experimented with feeding bits of dirt to a friendly currawong who would visit our place.
During the winter holidays, we would spend time at my grandparents’ farm to give them a well-earned break. Exploring the farm was like another world – we played with the piglets and the dairy cats, and learned about life-cycles and how we influence them. I recall poring over dad’s environmental science books and old National Geographic magazines; their glossy colour photographs fascinated me! Later, I was able to read the text of the familiar articles and soak up even more.
Still, something more substantial drew me toward Medicine.
Family anecdotes of more personal experiences with medical care would replay over and over in my mind. Mum had told me about my grandmother’s struggles with my uncle as a newborn, eventually leading to a diagnosis of WPW syndrome. They frequently travelled the 270 kilometres to the Royal Children’s Hospital (RCH) in Melbourne in the late ‘50s and ‘60s.
When I was a little older, my grandmother also told me about her own mother’s return to the farm with her little boy in the late 1930s. He had died at RCH of leukaemia, aged six, and she had travelled home with his body, alone, on the train. I couldn’t imagine the grief and hardship, let alone the added tyranny of distance.
It just didn’t seem right. I thought things needed to change, especially for the disadvantaged and the isolated.

With a young family (and two dachshunds) as well as their medical careers, life is busy for Erin and Ian!
What got you interested in Rural Medicine?
Erin: The doctors in Seymour – all RGs – had delivered my younger brother and sister. They were familiar and, to my child’s eyes, seemed to know ‘everything’. They inspired confidence and nothing my poor mother brought them (including her four unruly offspring) seemed to faze them. To top it off, they always gave us a jelly bean from the bottom drawer post consultation!
Ironically enough, my first foray with the wrong side of the law piqued my interest in Rural Medicine. I recall, perhaps around 7 years old, sneaking from bed of a night and hiding behind the lounge room wall. This vantage point allowed me to secretly watch Chris and Geoff in ‘The Flying Doctors’ and Terence and Shirley in ‘A Country Practice’. Their lives looked exciting and their relationships were central to achieving resolutions for everyone.
In real life, a decade later, an opportunity arose to spend a week of the Year 12 school holidays with Dr Peter Graham, the iconic rural doctor in the Victorian town of Cohuna (and later the namesake of the ACRRM-RDAA Peter Graham ‘Cohuna’ Award).
This planted the seed in my mind that something I had assumed was an idealised TV fantasy career was indeed a potential reality.
Ian: The turning point for me was a single weekend that Erin and I spent in Barham (on the NSW-Victorian border) with another FACRRM doctor.
We visited the home of Jolmer and Christel Smit (both RVTS alumni FACRRMs) and their five children, while Christel and their daughter were away overseas. Jolmer was on-call for the local hospital for the weekend but we had plenty of time for Jolmer and the four boys to take us picking apricots, milking cows at the neighbour’s farm, and making sausages (I was terrible at it!)
Our leisurely pursuits were put on hold with one phone call, however, and the weekend became a case study in how versatile and adaptable a Rural Generalist must be. It was the hospital triage nurse, informing Jolmer of the impending arrival of a farmer with a significant laceration to his foot, sustained operating an auger.
Jolmer asked us if we would be okay to help out (as larger hospital-based PGY3/4s) and we all made our way to the hospital – pretty briskly. What proceeded was not quite the ‘laceration’ initially described, but a complete above-ankle amputation from the teeth at the base of the auger shaft!
I was in awe of the way Jolmer concurrently performed the roles of rural emergency trauma doctor, team leader, pain team doctor and retrieval doctor.
Later, once our patient was safely transported to a nearby airfield for retrieval, the evening meal at the local Thai restaurant topped off the day’s events.
What towns have you worked in during your career?
Ian: I interned in Bendigo, later pursuing orthopaedic surgical training in Melbourne, before moving to Swan Hill and Kerang to complete my FACRRM training through RVTS.
Erin: My various clinical roles since completing my internship have all been based in Bendigo, Swan Hill or Kerang. Prior to working as a community and hospital-based Rural Generalist, I was an Emergency Medicine registrar training with ACEM and based in Bendigo.
What does your work mix now look like?
Ian: I work in Kerang and in Bendigo, doing a mix of GP and on-call for the Urgent Care Centre at the local hospital in Kerang, as well as emergency shifts fortnightly at Bendigo Hospital. I also assist surgeons with orthopaedic lists at the private hospital in Bendigo.
Erin: I work clinically on-call for the Urgent Care Centre at Kerang District Health, provide primary care at a residential aged care facility, and I’m a mentor to a Nurse Practitioner student.
What are the best bits about living and working in a rural community?
Immersion in the local community has been the most rewarding aspect of life in Kerang for both of us. We are a meaningful part of the local school, sporting club, childcare and social communities. We plan to be in Kerang for the long-term.
What have been your most amusing moments in Rural Medicine?
Walking around the local Woollies and reading our daughter’s school novels with her before bed in an N95 mask and industrial-strength goggles for the duration of the week before we went away on holidays…just in case the dreaded COVID bug visited our house!
And having to fix Erin’s nail-bed injury at two o’clock in the morning, while the kids were asleep, at the kitchen bench…her fingernail vs car door had caused an unbearably painful subungual haematoma, requiring a truly urgent ‘house call’!
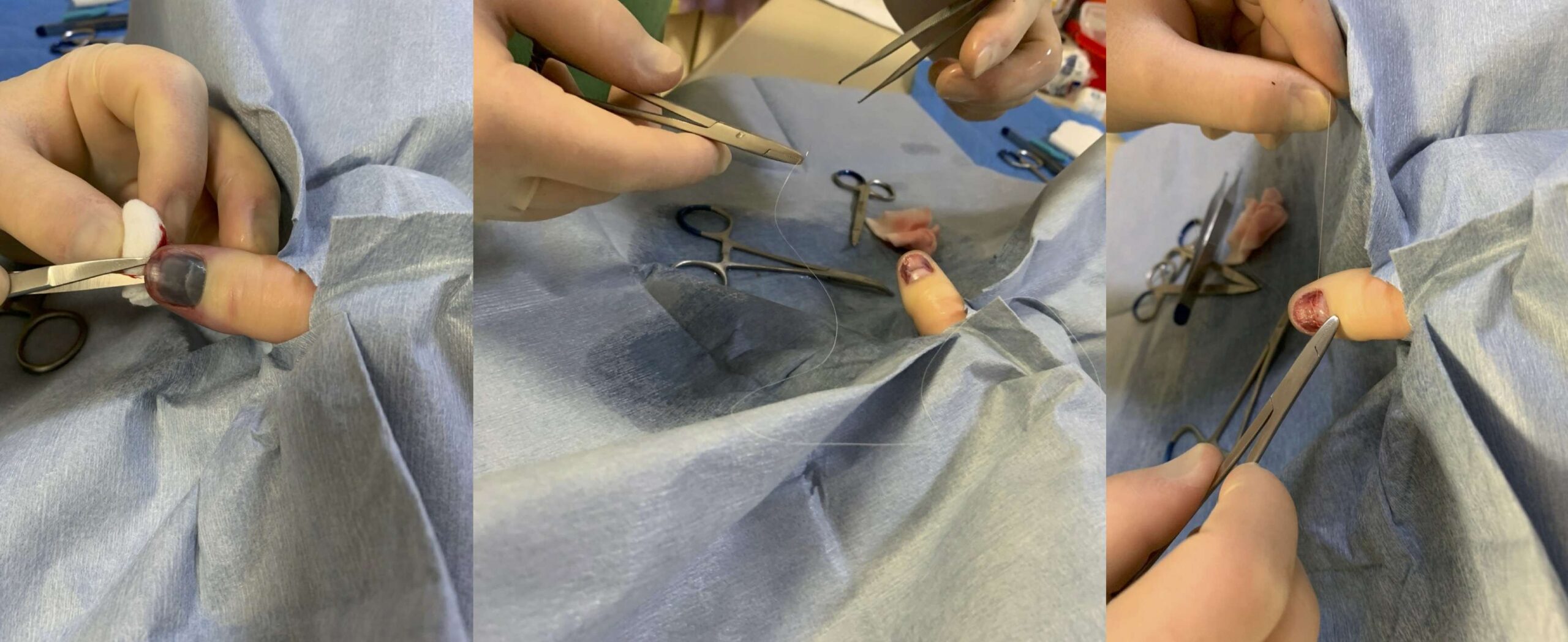
Car vs finger…
What have been the most special moments in Rural Medicine for you?
Nothing compares to the expressions of gratitude from patients and their families after we’ve provided care in times of serious sickness and/or dying. The opportunity to provide cradle-to-grave medical care to multiple members of a family – in sickness and in health – is a particular privilege.
What made RVTS a good option for your Rural Generalist training?
Erin: Our friendship with Jolmer and Christel was instrumental in guiding us towards the RVTS pathway from the very start. We weren’t even aware it existed until then, and AGPT was never a suitable option for us.
Our first baby was two-and-a-half years old when we applied to RVTS.
Training toward any Fellowship with a young (and expanding) family would always be a challenge, but RVTS shared our values and accommodated us with truly flexible training.
Medical post-graduate training is notoriously intolerant to accommodating the family lives of its trainees. We are immeasurably grateful to RVTS, where staff actively embrace family inclusion and cultural diversity. Ian and I could concurrently complete our training with RVTS in large part due to this inclusive approach.
Values we most appreciated included:
- RVTS prioritising its trainees remaining in rural location(s) as a condition of training – together, as a family! Strong community ties were positive for our family unit and for our community, allowing us to establish strong bonds.
- Family-friendly training events, including the week of funded workshops twice a year. The workshops were always socially and educationally excellent. We met other registrars and their families, and spent valuable time with our remote supervisors. As it happened, I was pregnant or breastfeeding for most of the workshops we attended.
- Educational system integrity:
- RVTS genuinely seeks and considers feedback from its registrars, educators and supervisors, and has inclusive and diverse representation at multiple levels of the organisation.
- RVTS educators openly acknowledge we are all learning with and from one another – humility, valuing the contribution of ideas and additional evidence, and relentless improvement are qualities that are always present.
- Supervision is available remotely and is adapted to the needs of each trainee.
- A can-do culture. This is by far the most important quality of RVTS and shapes its model of teaching, learning and function.
In addition to being an RVTS trainee, my involvement with RVTS as a Registrar Liaison Officer (RLO) provided insight into the multi-layered approach driving the organisation.
Why is RVTS important?
If the health of rural Australians is to improve appreciably, we must address workforce issues. The option to train with RVTS contributes to expansion, adequacy, retention and sustainability of our Rural Generalist workforce.
RVTS provides the most meaningfully appealing model we can envisage to achieve such progress – that is, an independent but simultaneously supported pathway with a family-friendly structure. Communities benefit, in real time, from the presence and service of RVTS RG/GP trainees (and their families) investing their professional and social capital as they qualify.
Add to that RVTS’s dedication to cultural awareness, safety, education and recognition, and the same could be said for its contribution to addressing the gap in actual health outcomes for our First Nations people.
What interests do you have outside Medicine?
Ian:
I have been a mad cricket fan since I can remember, but unfortunately don’t have the time to play at this stage in our lives. I have been involved in setting up our GP clinic as a Park Run practice to promote healthy lifestyles – this means participating in a weekly five kilometre walk/jog/run around the Kerang levy bank.
Erin:
Our stage of family life means leisure time requires conscious investment. I love crochet, and a good audiobook makes mundane housework more tolerable!
I’ve recently joined the local gym and am working on carving out time to make attending it more consistent. Our two dachshund puppies, Frankie and Penny, also keep us on our toes!





